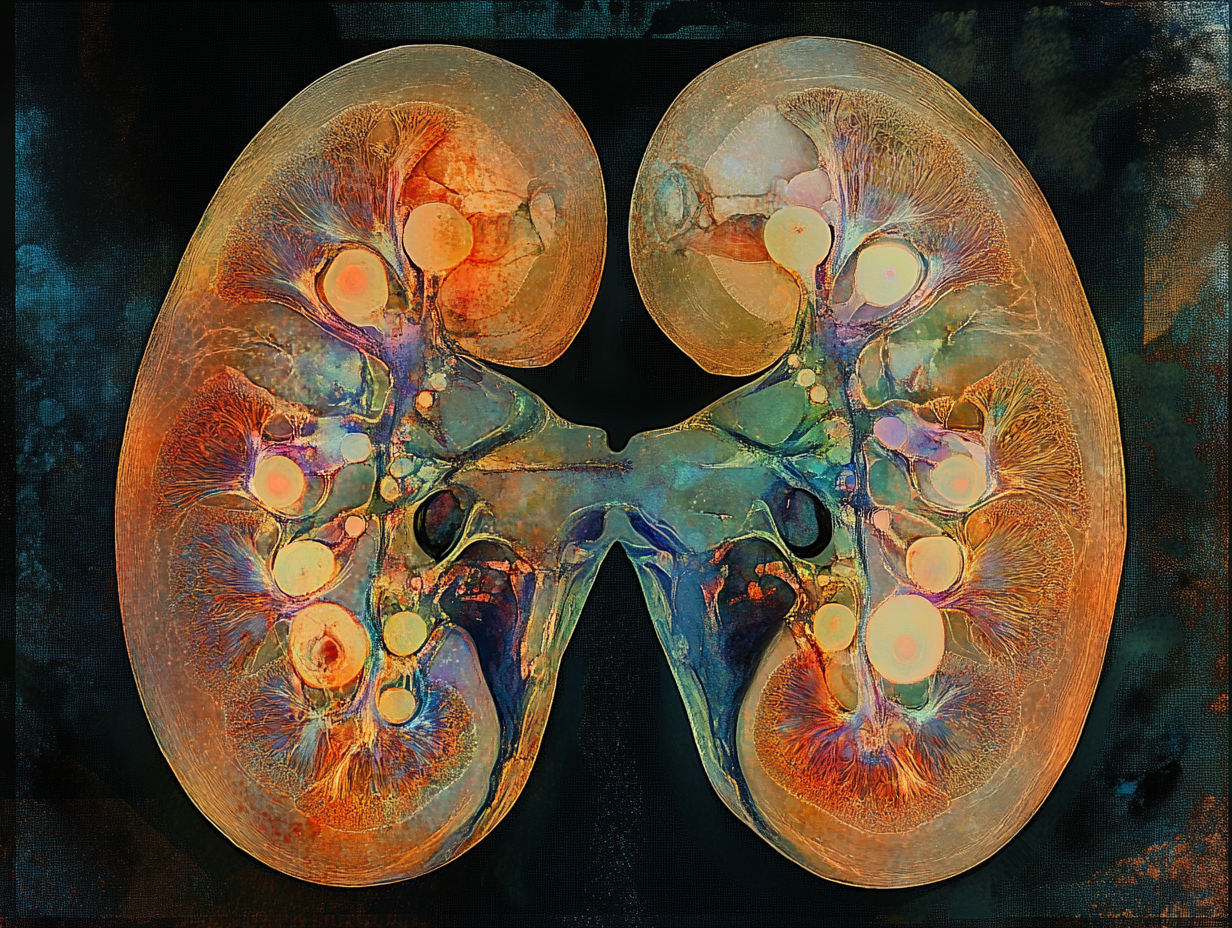
Basics of Kidney Function
The kidneys are two bean-shaped organs located on either side of the spine, just below the rib cage. Each kidney contains around one million tiny filtering units called nephrons, which are responsible for removing waste products and excess substances from the blood. This filtration process is vital for maintaining the body's fluid and electrolyte balance, regulating blood pressure, and ensuring the removal of metabolic waste.
The Filtration Process
The filtration process begins in the glomerulus, a network of capillaries within each nephron. Blood enters the glomerulus, where water, ions, and small molecules pass through the glomerular membrane into the Bowman's capsule, forming what is known as the filtrate. Larger molecules and blood cells remain in the bloodstream. This initial filtration is followed by reabsorption and secretion in the renal tubules, where essential substances like glucose, amino acids, and certain ions are reabsorbed back into the blood, and additional waste products are secreted into the filtrate to form urine.
Key Functions of the Kidneys
- Excretion of Waste Products: The kidneys remove urea, creatinine, and other metabolic by-products from the blood. Urea, produced from the breakdown of proteins, and creatinine, a by-product of muscle metabolism, are common waste products measured to assess kidney function.
- Regulation of Fluid and Electrolyte Balance: The kidneys regulate the body's fluid balance by adjusting the volume and concentration of urine. They also maintain the balance of electrolytes such as sodium, potassium, and calcium, which are crucial for nerve function, muscle contraction, and overall cellular function.
- Acid-Base Balance: By excreting hydrogen ions and reabsorbing bicarbonate, the kidneys help maintain the body's pH within a narrow range, which is essential for the proper functioning of enzymes and metabolic processes.
- Blood Pressure Regulation: The kidneys produce renin, an enzyme that plays a key role in the renin-angiotensin-aldosterone system (RAAS), which regulates blood pressure and fluid balance. Additionally, the kidneys respond to changes in blood pressure by adjusting the excretion of sodium and water.
- Erythropoiesis: The kidneys produce erythropoietin, a hormone that stimulates the production of red blood cells in the bone marrow. This function is crucial for maintaining adequate oxygen transport in the blood.
Common Kidney Function Tests
Serum Creatinine: Creatinine levels in the blood provide an estimate of kidney function. Normal levels typically range from 0.6 to 1.2 mg/dL in men and 0.5 to 1.1 mg/dL in women. Elevated creatinine levels indicate impaired kidney function or kidney disease. However, serum creatinine can be influenced by factors such as muscle mass, age, and sex, which may limit its accuracy.
Glomerular Filtration Rate (GFR): GFR is a measure of how much blood the kidneys filter per minute. The normal GFR for a healthy adult is approximately 90-120 mL/min/1.73 m². GFR can be estimated using formulas that incorporate serum creatinine levels, age, sex, and body size. A decline in GFR indicates a reduction in kidney function, and GFR values below 60 mL/min/1.73 m² for three months or more are indicative of chronic kidney disease (CKD).
Limitations of Traditional Tests
While serum creatinine and GFR are widely used, they have limitations. Serum creatinine levels can be affected by non-renal factors, such as diet, muscle mass, and certain medications. Additionally, GFR estimates based on creatinine may not be accurate in all populations, including the elderly and those with muscle wasting conditions. These limitations highlight the need for more reliable biomarkers, such as Cystatin C, to improve the assessment of kidney function.
What is Cystatin C?
Definition and Role
Cystatin C is a small protein produced by all nucleated cells in the body and plays a crucial role in regulating the activity of cathepsins, enzymes involved in protein degradation. Unlike serum creatinine, Cystatin C is produced at a constant rate by all nucleated cells, making it a reliable marker for assessing kidney function.
Production and Elimination
Cystatin C is continuously produced and released into the bloodstream. It is freely filtered by the glomeruli in the kidneys and almost entirely reabsorbed and catabolized by the renal tubules. Because it is not secreted by the renal tubules and its production is relatively constant, Cystatin C levels in the blood provide a more accurate reflection of the glomerular filtration rate (GFR) compared to serum creatinine.
Advantages Over Creatinine
One of the significant advantages of Cystatin C is its independence from factors that affect creatinine levels. Serum creatinine is influenced by muscle mass, age, sex, and diet, which can lead to variability in its accuracy as a biomarker for kidney function. In contrast, Cystatin C levels are not significantly affected by muscle mass or diet, making it a more reliable indicator of kidney function across different populations, including the elderly and those with muscle wasting conditions.
Clinical Studies and Data
Research has demonstrated the superior accuracy of Cystatin C in estimating GFR. A study published in the New England Journal of Medicine found that eGFR based on Cystatin C alone or combined with creatinine provides a more accurate assessment of kidney function than creatinine alone, especially in older adults (Inker et al., 2012). Another study showed that Cystatin C-based eGFR is a better predictor of cardiovascular events and mortality in patients with chronic kidney disease (CKD) compared to creatinine-based eGFR (Shlipak et al., 2013).
Applications in Clinical Practice
Cystatin C is particularly useful in situations where creatinine-based GFR estimates are less reliable. For example, in elderly patients or those with low muscle mass, Cystatin C provides a more accurate measure of kidney function. Additionally, Cystatin C can be beneficial in detecting early-stage kidney disease, as its levels increase earlier than creatinine in the course of kidney dysfunction.
Measuring Cystatin C
Cystatin C levels can be measured using immunoassays, such as nephelometry or turbidimetry. The reference range for Cystatin C in healthy adults is approximately 0.6 to 1.2 mg/L. Elevated levels indicate impaired kidney function and necessitate further evaluation and monitoring.
Understanding eGFR
Estimated Glomerular Filtration Rate (eGFR) is a crucial measure used to assess how well the kidneys are filtering blood. It estimates the rate at which the glomeruli, the tiny filters in the kidneys, remove waste products from the blood. A normal eGFR is typically between 90 and 120 mL/min/1.73 m². An eGFR below 60 mL/min/1.73 m² for three months or more is indicative of chronic kidney disease (CKD).
Reference Ranges
≥ 90 mL/min/1.73 m²: Normal kidney function. However, even with a normal eGFR, if there are other signs of kidney damage, further investigation is needed.
60-89 mL/min/1.73 m²: Mildly decreased kidney function. This may be normal for some people, especially the elderly, but it can also indicate early kidney disease.
30-59 mL/min/1.73 m²: Moderately decreased kidney function, indicating Stage 3 CKD.
15-29 mL/min/1.73 m²: Severely decreased kidney function, indicating Stage 4 CKD.
< 15 mL/min/1.73 m²: Kidney failure, indicating Stage 5 CKD, which typically requires dialysis or a kidney transplant.
How to lower Cystatin C?
While Cystatin C levels primarily reflect kidney health, they can be influenced by various factors. Here are some strategies to help lower Cystatin C levels:
1. Manage Underlying Conditions
Hypertension:
- Control Blood Pressure: Keeping blood pressure within the target range (usually below 140/90 mmHg) can help reduce kidney strain. Medications such as ACE inhibitors or angiotensin II receptor blockers (ARBs) are often prescribed to help manage blood pressure and protect kidney function.
- Lifestyle Changes: Reducing salt intake, losing weight, and engaging in regular physical activity can also help lower blood pressure.
Diabetes:
- Glycemic Control: Maintaining blood glucose levels within the target range can prevent further kidney damage. This includes taking prescribed medications, monitoring blood sugar levels, and following a balanced diet.
- Regular Monitoring: Regularly checking kidney function and working closely with a healthcare provider to adjust treatment plans as necessary.
2. Dietary Adjustments
Reduce Protein Intake:
- Moderate Protein Consumption: While protein is essential for health, excessive intake can strain the kidneys. Consult a dietitian to determine the appropriate amount of protein for your condition.
Balanced Diet:
- Healthy Eating: A diet rich in fruits, vegetables, whole grains, and lean proteins supports overall kidney health. The DASH (Dietary Approaches to Stop Hypertension) diet is often recommended for individuals with kidney concerns.
- Limit Sodium: High sodium intake can elevate blood pressure and worsen kidney function. Aim to consume less than 2,300 mg of sodium per day.
Reduce Phosphorus and Potassium:
- Monitor Intake: If kidney function is impaired, managing phosphorus and potassium intake is crucial. Foods high in phosphorus include dairy products, nuts, and beans, while high-potassium foods include bananas, oranges, and potatoes.
3. Lifestyle Changes
Regular Exercise:
- Stay Active: Engage in at least 150 minutes of moderate-intensity exercise per week, such as brisk walking or cycling. Exercise helps improve cardiovascular health and can support kidney function.
Weight Management:
- Achieve a Healthy Weight: Maintaining a healthy weight can reduce the strain on your kidneys. Aim for a BMI within the normal range (18.5-24.9).
Quit Smoking:
- Avoid Tobacco: Smoking can worsen kidney function and increase the risk of cardiovascular disease. Quitting smoking can improve overall health and potentially lower Cystatin C levels.
4. Medication Management
Review Medications:
- Avoid Nephrotoxic Drugs: Some medications can harm the kidneys. Work with your healthcare provider to review all medications and avoid those that can negatively impact kidney function.
- Adhere to Prescribed Treatments: Follow your healthcare provider's recommendations for managing any underlying conditions that can affect kidney health.
Lowering Cystatin C levels involves a comprehensive approach that includes managing underlying conditions, making dietary adjustments, adopting a healthy lifestyle, reviewing medications, and maintaining regular medical follow-up.
Conclusion
Cystatin C serves as a valuable biomarker not only for assessing kidney function but also for providing insights into cardiovascular health and overall mortality risk. Elevated levels of Cystatin C are associated with an increased risk of cardiovascular events and all-cause mortality, making it an important marker for predicting longevity. TeleTest offers Cystatin C testing as part of our longevity panel. By monitoring Cystatin C levels, healthcare providers can gain a better understanding of an individual's health status and implement early interventions to improve long-term outcomes.
Disclaimer: This blog post is intended for educational purposes only and should not be taken as medical advice. Always consult your healthcare provider for personal health concerns.