Understanding GLP-1
The glucagon-like peptide-1 (GLP-1) hormone is a multifaceted component of the body’s intricate system for regulating blood sugar. Originating primarily in the intestines, GLP-1 is released into the bloodstream in response to food intake. But GLP-1 does more than just respond passively—it actively participates in managing the body's metabolic processes.
When food enters the digestive system, GLP-1 is secreted by cells in the gut known as L-cells. This release is a signal to the body, particularly the pancreas, that nutrients are on their way. The pancreas, in turn, begins preparing to release insulin, the hormone responsible for lowering blood sugar levels by allowing cells to absorb glucose from the blood.
However, the role of GLP-1 goes beyond merely triggering insulin production. It also inhibits the release of glucagon, another hormone produced by the pancreas that has the opposite effect of insulin—it raises blood sugar levels by signaling the liver to release stored glucose. By suppressing glucagon, GLP-1 ensures that blood sugar levels do not spike excessively after a meal.
Moreover, GLP-1 has a hand in how food is processed in the digestive system. It slows the rate at which the stomach empties its contents into the small intestine, which results in a more gradual absorption of glucose into the bloodstream. This not only helps prevent sudden increases in blood sugar but also contributes to a feeling of fullness, which can reduce overall food intake.
GLP-1 and Blood Sugar Regulation
GLP-1 plays a pivotal role in fine-tuning the body's response to food intake, acting as a multifaceted hormone that influences several critical aspects of blood sugar regulation. This section delves into the specific mechanisms through which GLP-1 helps maintain blood sugar balance, offering a closer look at its direct impact on insulin, glucagon, and the digestive process.
- Enhanced Insulin Secretion: One of the primary actions of GLP-1 is its ability to enhance insulin secretion in response to rising blood sugar levels. After a meal, as glucose enters the bloodstream, GLP-1 amplifies the pancreas’s response, ensuring that more insulin is released to help cells absorb glucose efficiently. This action is glucose-dependent, meaning GLP-1 increases insulin secretion only when blood sugar levels are elevated, which helps to prevent hyperglycemia (when blood sugar gets too high).
- Inhibition of Glucagon Release: While insulin lowers blood sugar, glucagon has the opposite effect, raising it by signaling the liver to release stored glucose. GLP-1 suppresses this glucagon release, particularly when blood sugar levels are high, preventing the liver from adding more glucose to the bloodstream. This coordinated effort between GLP-1 and insulin ensures that blood sugar levels remain within a healthy range after eating, avoiding the spikes that can lead to long-term health issues.
- Slowing Gastric Emptying: GLP-1 also plays a crucial role in the digestive process by slowing down gastric emptying, which is the rate at which food leaves the stomach and enters the small intestine. By delaying this process, GLP-1 helps to moderate the release of glucose into the bloodstream, leading to a more gradual and sustained increase in blood sugar levels. This slower absorption not only prevents sudden spikes in blood sugar but also extends the feeling of fullness, potentially reducing overall caloric intake and supporting weight management.
- Appetite Regulation and Satiety: Beyond its direct impact on blood sugar, GLP-1 influences appetite by promoting satiety, or the feeling of fullness, after eating. This effect is partly due to its action on the central nervous system, where GLP-1 receptors in the brain help regulate hunger signals. By enhancing the sensation of fullness, GLP-1 can help individuals control their food intake, which is particularly beneficial for those managing weight or dealing with conditions like obesity, where overeating can exacerbate blood sugar imbalances.
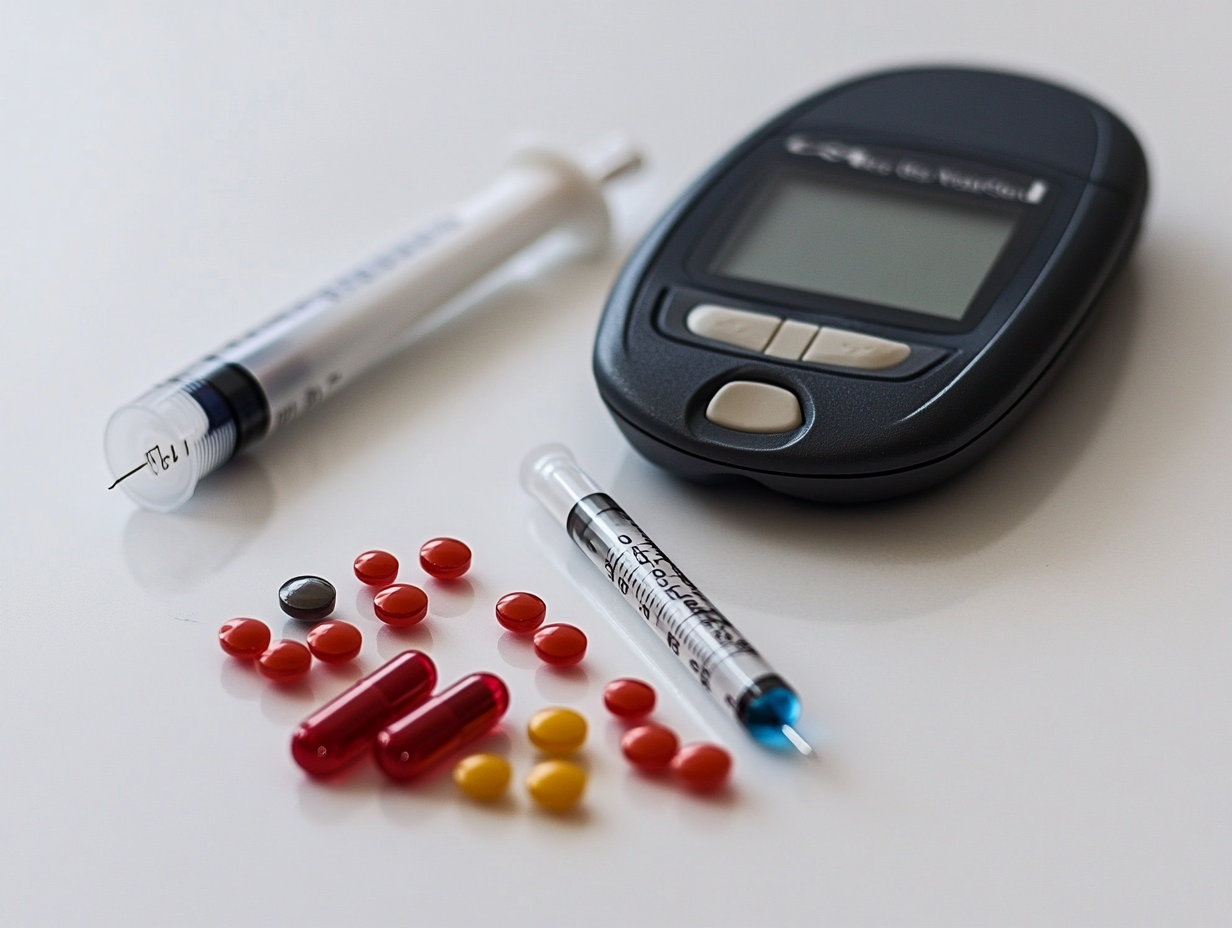
The Role of GLP-1 in Diabetes Management
For individuals with Type 2 diabetes, maintaining stable blood sugar levels is a constant challenge. GLP-1 has emerged as a powerful ally in this battle, not only through its natural functions in the body but also via pharmaceutical advancements that harness its capabilities. This section explores the therapeutic role of GLP-1 in managing diabetes, particularly focusing on GLP-1 agonists, a class of medications that mimic the hormone’s effects.
- Introduction to GLP-1 Agonists: GLP-1 agonists are a relatively new class of medications that have transformed the landscape of Type 2 diabetes treatment. These drugs work by mimicking the action of natural GLP-1, thereby enhancing its beneficial effects on blood sugar regulation. Unlike other diabetes medications that stimulate insulin release indiscriminately, GLP-1 agonists do so in a glucose-dependent manner, reducing the risk of hypoglycemia (dangerously low blood sugar levels) .
- Effectiveness in Glycemic Control: Studies have shown that GLP-1 agonists are highly effective in lowering HbA1c levels, a key marker of long-term blood sugar control. By improving both fasting and postprandial (after eating) blood sugar levels, GLP-1 agonists help patients achieve better overall glycemic control. This improved control is critical in preventing the complications of diabetes, such as neuropathy, nephropathy, and retinopathy, which are particularly prevalent in long-term, poorly managed diabetes.
- Additional Health Benefits: Beyond blood sugar control, GLP-1 agonists offer additional health benefits, particularly concerning weight management and cardiovascular health. Many patients on GLP-1 agonists experience significant weight loss, which is a crucial factor in managing Type 2 diabetes. This weight loss is largely attributed to the hormone’s appetite-suppressing effects, which help reduce caloric intake.
Moreover, GLP-1 agonists have been associated with reduced cardiovascular risk, an essential consideration since individuals with Type 2 diabetes are at a higher risk for heart disease. Some GLP-1 agonists have been shown to lower the risk of major adverse cardiovascular events, such as heart attacks and strokes, making them a valuable tool in comprehensive diabetes care.
- Integration into Diabetes Treatment Plans: GLP-1 agonists are typically used as part of a broader diabetes management plan, which may include other medications, lifestyle changes, and regular monitoring of blood sugar levels. They are often prescribed when other treatments, such as metformin, are not sufficient to achieve target blood sugar levels. Healthcare providers tailor the use of GLP-1 agonists to each patient’s specific needs, considering factors such as the severity of diabetes, weight management goals, and cardiovascular health.
- Availability and Accessibility in Canada: In Canada, GLP-1 agonists are available by prescription and are covered by many provincial drug plans and private insurance policies, though coverage may vary. Given their benefits, these medications have become an increasingly popular choice for managing Type 2 diabetes. However, their cost can be a consideration, particularly for patients without comprehensive insurance coverage. It's important for Canadian patients to discuss the availability and affordability of these treatments with their healthcare providers.
GLP-1 and the Canadian Healthcare System
As GLP-1 agonists gain prominence in the treatment of Type 2 diabetes, understanding their role within the Canadian healthcare system is crucial. This section will explore the accessibility, cost, and the role healthcare providers play in ensuring that patients benefit from these advanced treatments.
- Accessibility of GLP-1 Agonists in Canada: GLP-1 agonists are available across Canada, but access can vary depending on several factors, including provincial healthcare policies, availability of insurance coverage, and whether a patient lives in an urban or rural area. Most provinces include GLP-1 agonists in their drug formularies, meaning they are covered under provincial healthcare plans for those who qualify. However, the process of getting coverage may require meeting specific criteria, such as proving that other diabetes treatments have been ineffective.
For those without provincial coverage, private insurance often plays a critical role. Most major insurance providers in Canada cover GLP-1 agonists, but patients may face co-pays or other out-of-pocket expenses depending on their specific insurance plan.
See here for prices without insurance.
- The Role of Healthcare Providers: Healthcare providers, including family doctors, endocrinologists, and diabetes educators, are at the forefront of managing diabetes care in Canada. Their role in prescribing and monitoring the use of GLP-1 agonists is vital. Providers must carefully evaluate each patient’s health status, history, and treatment goals before recommending GLP-1 agonists. This evaluation often includes considering the patient’s cardiovascular risk, potential benefits of weight loss, and the need for improved glycemic control.
Additionally, providers play a key role in educating patients about the proper use of GLP-1 agonists, including how to administer the medication (often via injection), manage potential side effects, and monitor blood sugar levels. Regular follow-ups are essential to assess the efficacy of the treatment and make any necessary adjustments.
- Financial Considerations and Support Programs: While GLP-1 agonists offer significant health benefits, their cost can be a barrier for some Canadians, especially those without comprehensive insurance coverage. The cost of these medications can range significantly depending on the brand and dosage, leading some patients to seek financial assistance.
To address this, several pharmaceutical companies offer patient support programs that provide financial aid, often in the form of discounts or payment plans, to make these medications more affordable. Additionally, some provinces offer special programs for low-income patients or those with significant health needs, ensuring broader access to essential treatments.
Patients are encouraged to speak with their healthcare providers about these options and to explore all available avenues for financial support. In many cases, a combination of provincial healthcare coverage, private insurance, and manufacturer assistance can help reduce the financial burden.
- Future Outlook: As research continues to support the benefits of GLP-1 agonists, it is likely that their role in the Canadian healthcare system will expand. Ongoing clinical trials and real-world studies may lead to broader indications for their use, potentially making these medications available to a wider range of patients, including those with prediabetes or those at high cardiovascular risk.
Moreover, as the cost of GLP-1 agonists decreases over time, we may see more inclusive policies that provide greater access across all demographics, including those who currently face financial or geographical barriers.
The integration of GLP-1 agonists into the Canadian healthcare system represents a significant step forward in the management of Type 2 diabetes. By ensuring that these medications are accessible and affordable, and by leveraging the expertise of healthcare providers, Canada is positioning itself to offer better health outcomes for diabetes patients nationwide.
Lifestyle Considerations
While GLP-1 agonists and other medical treatments are essential tools in managing Type 2 diabetes, lifestyle choices play a critical role in optimizing their effectiveness. This section explores how diet, exercise, and other lifestyle factors can complement GLP-1-based therapies, helping Canadians achieve better blood sugar control and overall health outcomes.
- Diet and Nutrition: The foods you eat can significantly impact the effectiveness of GLP-1 agonists in regulating blood sugar levels. A balanced diet rich in whole grains, lean proteins, healthy fats, and plenty of fruits and vegetables is crucial. These foods help stabilize blood sugar levels and work synergistically with GLP-1’s natural effects, such as slowing gastric emptying and reducing postprandial glucose spikes.
Additionally, incorporating foods that are high in fiber, such as legumes, oats, and certain fruits, can further support the hormone's function by promoting satiety and slowing the absorption of glucose. Canadians are encouraged to follow dietary guidelines that emphasize nutrient-dense foods and to avoid excessive consumption of refined sugars and processed foods, which can counteract the benefits of GLP-1 agonists.
- Exercise and Physical Activity: Regular physical activity is another cornerstone of effective diabetes management, particularly when combined with GLP-1 agonists. Exercise enhances the body's sensitivity to insulin, which complements the GLP-1-mediated increase in insulin secretion. Activities such as brisk walking, cycling, and strength training can help lower blood sugar levels both immediately and over time.
Moreover, exercise contributes to weight management, which is a key benefit of GLP-1 therapy. For many Canadians, achieving and maintaining a healthy weight can improve both blood sugar control and cardiovascular health, reducing the overall risk of diabetes complications.
- Stress Management: Chronic stress can interfere with blood sugar regulation, making it more challenging to achieve optimal control. High stress levels can trigger the release of hormones like cortisol, which increases blood sugar levels. Integrating stress management techniques such as mindfulness meditation, deep breathing exercises, or yoga can help reduce stress and support the body’s natural blood sugar regulation processes.
Additionally, sufficient sleep is crucial in managing stress and maintaining hormonal balance, including the balance of insulin and GLP-1. Canadians should aim for 7-9 hours of quality sleep per night to support their overall health and enhance the effectiveness of their diabetes treatment plan.
- Monitoring Blood Sugar Levels: Regular monitoring of blood sugar levels is essential for anyone using GLP-1 agonists, as it provides valuable feedback on how well the treatment is working. Keeping track of blood sugar readings before and after meals can help identify patterns and inform adjustments in diet, activity, or medication.
For those using continuous glucose monitors (CGMs), real-time data can provide insights into how lifestyle factors such as diet, exercise, and stress affect blood sugar levels throughout the day. This information can be used to make informed decisions about lifestyle changes that can improve glycemic control.
Conclusion
The role of GLP-1 in regulating blood sugar is multifaceted and crucial for individuals managing Type 2 diabetes, particularly in the Canadian context where access to innovative treatments like GLP-1 agonists is increasingly widespread. By influencing insulin secretion, inhibiting glucagon release, slowing gastric emptying, and promoting satiety, GLP-1 acts as a powerful regulator of glucose metabolism, offering both direct and indirect benefits that extend beyond blood sugar control.
For Canadians, understanding how GLP-1 functions and how it can be harnessed through medication and lifestyle changes is essential. The availability of GLP-1 agonists provides a valuable tool in the ongoing management of diabetes, and when combined with a balanced diet, regular exercise, and proper stress management, these treatments can significantly enhance quality of life and health outcomes.
As the medical community continues to explore and expand the uses of GLP-1 therapies, the potential for improving diabetes care grows. For those living with diabetes in Canada, staying informed about these advancements and working closely with healthcare providers to tailor treatment plans is key to achieving optimal health.
Whether you’re considering GLP-1 agonists for the first time or are looking to maximize their benefits through lifestyle adjustments, the path to better blood sugar control is within reach. The future of diabetes management is promising, and with the right tools and knowledge, Canadians can navigate this journey with confidence and hope.
Disclaimer: This blog post is intended for educational purposes only and should not be taken as medical advice. Always consult your healthcare provider for personal health concerns.