Does OHIP cover Prescription Medication?
Short answer: it depends. As of 2018, Ontario expanded its medicare program, known as Ontario Drug Benefit (ODB) that covers the cost of most prescriptions for everyone under the age of 25 or those who are 65 are not already covered by a private plan. You may also qualify if you are living in a long-term care home, home for special care, or Community Home for Opportunity, as well as those receiving professional home and community care services or benefits from Ontario Works and Ontario Disability Support Program.
You do not have to enroll but coverage stops on your 25th birthday. Then on the first day of the month after you turn 65 years old, you’ll be automatically enrolled back in ODB.
So good news if you have children or you yourself are under 25 years old or 65 and over, most drugs are free.
What drugs are covered?
While you may meet the age requirement, not all drugs are covered. The easiest way to see if the drug you need is covered is by checking here. You can search by brand name, ingredient or generic name, its drug identification number (DIN), or sometimes even by its therapeutic use.
For example, if you were curious if birth control pills were covered, you can simply type “birth control.”
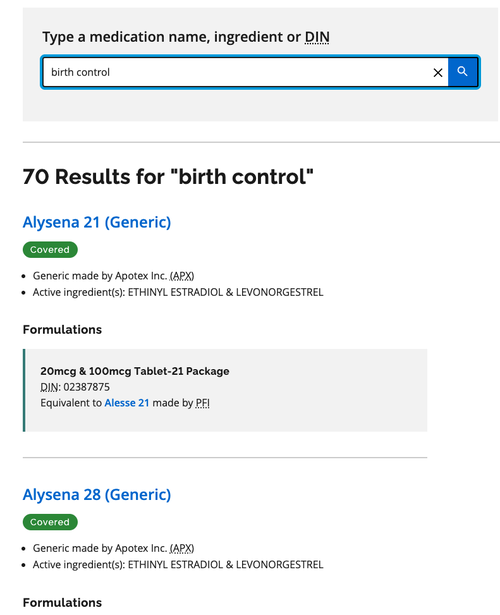
As you can see, 70 formulations across various brands and manufacturers are in fact covered.
Limited Use
Certain drugs are only covered under specific medical circumstances.

As you can see, if you search for “Ozempic,” it’s labeled as a “Limited Use” medication and “May be covered” under specific conditions. Unfortunately Ontario.ca does not show the specific conditions, but you can see the details if you perform a formulary search.
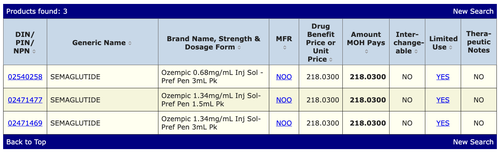
When you click “YES” under the “Limited Use” column, you can see the specific conditions that's required for coverage.
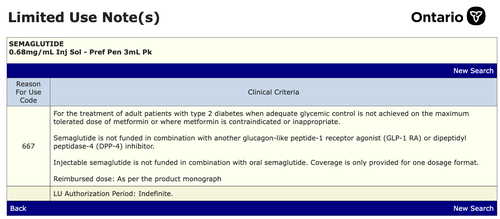
For Ozempic, only patients diagnosed with type 2 diabetes, along with other criteria, are covered.
Exceptional Access Program
There is an additional program which may help cover the cost of medication on a case-by-case basis that you can apply for with this form.
Private Insurance
If you are between the ages of 25 and 64 and do not qualify for the Ontario Drug Benefit program, some employers offer private insurance plans that may cover the cost of specific medications.
Here are some steps you can take to find out if your specific plan covers these medications:
- Review Your Insurance Policy: Start by looking at the details of your health insurance policy. Most insurers provide a list of covered medications, also known as a formulary, which you can often find on their website or by calling customer service.
- Contact Your Insurance Provider: To get the most accurate information, call your insurance provider directly. Ask them about coverage for the specific weight loss medication you are considering, such as semaglutide, tirzepatide, or liraglutide. Be sure to inquire about any conditions or criteria that must be met for coverage.
Similar to the limited use codes of the Ontario Drug Benefit program, some insurance plans have specific rules about what medications they will cover based on the conditions for which the drugs were originally approved (On-label vs. Off-label Use) by regulatory agencies such as Health Canada.
Here's a breakdown of what that means:
- On-label use refers to the use of a medication for conditions for which it was specifically approved. These are the uses that have been thoroughly reviewed and approved by regulatory bodies after clinical trials demonstrate the drug's safety and effectiveness for those conditions. Saxenda (Liraglutide) and Wegovy (semaglutide) are both officially approved for weight loss
- Off-label use involves prescribing medications for conditions other than those for which it was originally approved. This practice is legal and common, often based on emerging research or clinical experience suggesting the medication's effectiveness for other conditions. However, insurance companies may not always cover off-label uses because these uses lack formal regulatory approval. Mounjaro (Tirzepatide) and Ozempic (semaglutide) are not officially approved for weight loss, but are approved for diabetes
Some insurance providers will only reimburse or cover the cost of the medication if you meet the 'on-label' prescribing criteria. A physician during your consultation can help you select the appropriate medication depending on your coverage.
Paying Out-of-Pocket
If neither OHIP nor private insurance covers the medication you need, you may still opt to pay for your prescription out-of-pocket. You can see a list of common medications and typical prices you can expect to pay here.
Disclaimer: This blog post is intended for educational purposes only and should not be taken as medical advice. Always consult your healthcare provider for personal health concerns.
