Understanding Hormones and Hormone Therapy
What are Hormones?
Hormones are chemical messengers produced by glands in the endocrine system. They travel through the bloodstream to various organs and tissues, regulating numerous bodily functions such as metabolism, growth, mood, and reproductive processes. Hormones play a crucial role in maintaining homeostasis, and their balance is vital for overall health.
Common hormones involved in hormone therapy include:
- Estrogen: Primarily involved in the regulation of the female reproductive system and secondary sexual characteristics. It is essential for menstrual cycle regulation and bone health.
- Testosterone: The primary male sex hormone, responsible for the development of male physical characteristics, muscle mass, and libido. It is also important for women’s health, influencing mood and energy levels.
- Progesterone: This hormone prepares the uterus for pregnancy and regulates the menstrual cycle. It plays a crucial role in maintaining pregnancy and overall reproductive health.
Types of Hormone Therapy
Hormone therapy can be categorized into several types based on the hormones involved and the conditions being treated. Here’s an overview of the most common options:
- Estrogen Therapy: Often used to alleviate symptoms of menopause, such as hot flashes and vaginal dryness. It can be administered in various forms, including oral pills, transdermal patches, gels, and vaginal creams.
- Testosterone Therapy: Typically prescribed for individuals with low testosterone levels, this therapy can enhance energy, mood, and sexual function. Delivery methods include injections, patches, gels, and pellets.
- Combined Hormone Therapy: This approach involves the administration of both estrogen and progesterone (or progestin) to balance the effects of estrogen, especially in women who have not had a hysterectomy. It is commonly used to manage menopausal symptoms while minimizing the risk of endometrial cancer.
Indications for Hormone Therapy
Hormone therapy is indicated for various conditions and symptoms, including:
- Menopause and Perimenopause: Women experiencing significant discomfort from menopausal symptoms—such as hot flashes, night sweats, and mood swings—often benefit from hormone therapy. This treatment can provide relief and improve overall quality of life.
- Gender Dysphoria and Transition: Individuals undergoing gender transition may seek hormone therapy to align their physical characteristics with their gender identity. This can include testosterone therapy for transgender men and estrogen therapy for transgender women.
- Hypogonadism and Other Hormonal Imbalances: Conditions that result in insufficient hormone production, such as hypogonadism, can be managed with hormone therapy. This therapy aims to restore hormonal levels to a normal range, alleviating symptoms and improving health outcomes.
Understanding the fundamental roles of hormones and the types of hormone therapies available sets the stage for recognizing the importance of monitoring these therapies through blood tests, which we will explore in the next section.
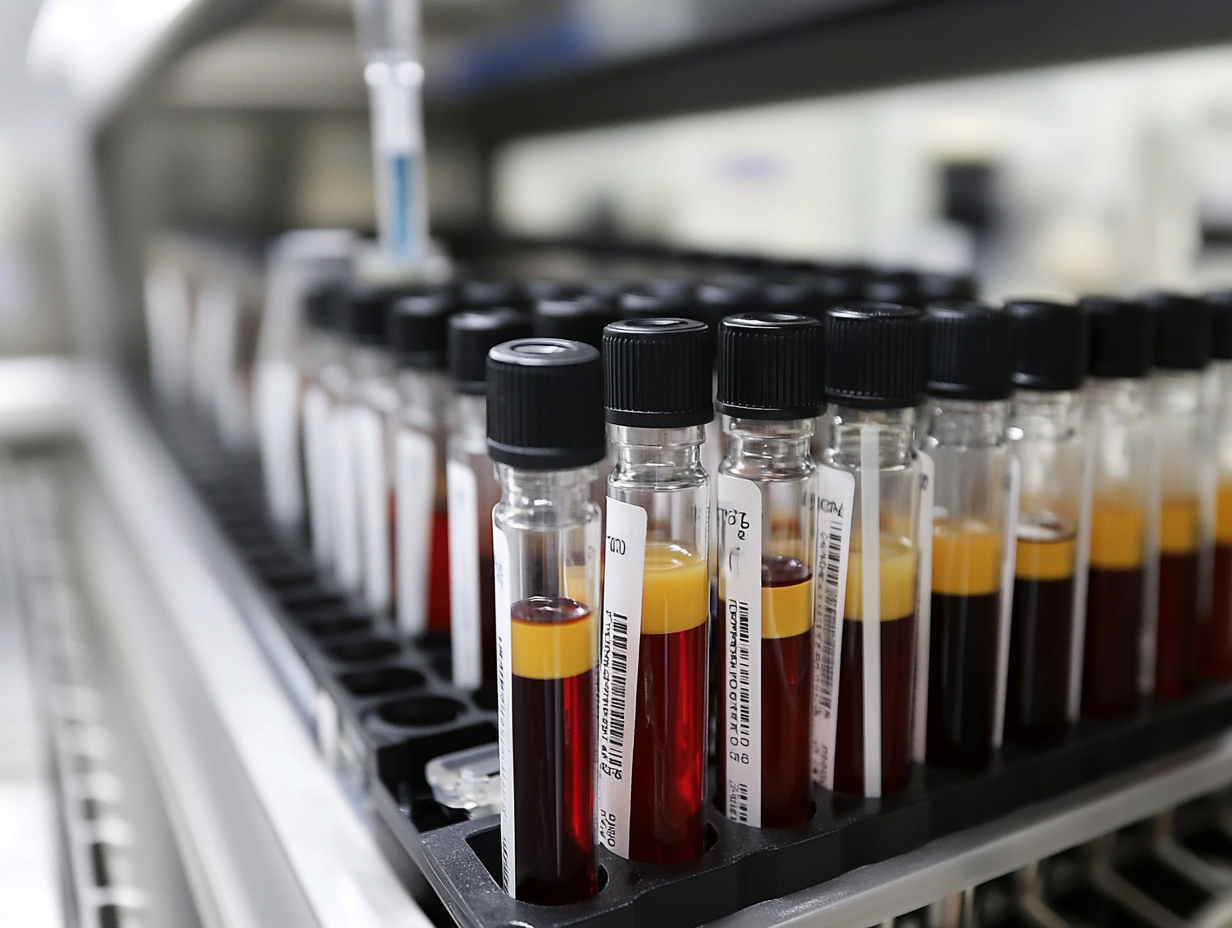
The Importance of Blood Test Monitoring
What Blood Tests are Commonly Used?
Blood tests play a critical role in monitoring the effectiveness and safety of hormone therapy. They help healthcare providers assess hormone levels and adjust treatments accordingly. Here are some of the key blood tests commonly used in hormone therapy monitoring:
- Estradiol Levels: This test measures the level of estradiol, the primary form of estrogen in the body. Monitoring estradiol is essential for women undergoing estrogen therapy, particularly to ensure that levels are adequate to alleviate menopausal symptoms without increasing the risk of adverse effects.
- Testosterone Levels: For individuals receiving testosterone therapy, regular monitoring of testosterone levels is crucial. This helps to ensure that levels are within the desired range, enhancing benefits like improved energy and mood while minimizing potential side effects.
- Progesterone Levels: This test is particularly important for women on combined hormone therapy. Monitoring progesterone helps assess the balance between estrogen and progesterone, which is vital for reducing the risk of endometrial hyperplasia and other complications.
- Thyroid Function Tests: Since thyroid hormones can influence overall hormonal balance and metabolism, these tests are often included in routine monitoring to rule out thyroid-related issues that could impact hormone therapy outcomes.
- Complete Blood Count (CBC): A CBC is important to monitor overall health and detect any potential side effects of hormone therapy, such as changes in blood cell counts which might indicate complications like blood clots.
How Blood Tests Inform Treatment
Establishing a baseline measurement before initiating hormone therapy is a standard practice. This initial assessment helps healthcare providers understand a patient’s starting hormone levels and tailor the therapy accordingly. Regular monitoring of hormone levels through blood tests serves several purposes:
- Assessing Hormone Levels: Blood tests provide critical information about how well the body is responding to hormone therapy. They can indicate whether hormone levels are too low, too high, or within the optimal range.
- Adjusting Therapy: Based on blood test results, healthcare providers may adjust dosages, change delivery methods, or even switch hormone formulations. This personalized approach maximizes therapeutic benefits while minimizing risks.
- Tracking Progress: Regular blood tests allow for ongoing evaluation of treatment efficacy. For instance, if a patient’s symptoms persist despite therapy, adjustments can be made based on test results, ensuring a more effective management of symptoms.
Risks of Not Monitoring
Neglecting to monitor hormone levels during therapy can lead to significant health risks and complications:
- Hormonal Imbalances: Without regular monitoring, patients may experience hormonal imbalances that can manifest as severe side effects, such as mood swings, weight gain, or increased anxiety.
- Increased Risk of Blood Clots: Certain hormone therapies, particularly those involving estrogen, may increase the risk of blood clots. Regular blood testing helps assess this risk and allows for timely interventions.
- Negative Impacts on Overall Health: Failure to monitor can lead to untreated hormonal deficiencies or excesses, which can adversely affect numerous bodily systems, including cardiovascular health, bone density, and mental well-being.
In summary, blood test monitoring is an essential component of hormone therapy, ensuring that treatment is safe and effective. It empowers both patients and healthcare providers to make informed decisions, ultimately leading to better health outcomes. In the next section, we will delve into interpreting blood test results and understanding what they mean for your treatment plan.
Interpreting Blood Test Results
Understanding Normal Ranges
Interpreting blood test results is a crucial aspect of managing hormone therapy. Normal hormone levels can vary significantly depending on several factors, including age, sex, and individual health circumstances.
- Estradiol Levels: For women, normal estradiol levels typically range from 15 to 350 picograms per milliliter (pg/mL) depending on the phase of the menstrual cycle. In postmenopausal women, levels generally fall below 30 pg/mL.
- Testosterone Levels: Normal testosterone levels in adult males usually range from 300 to 1,000 nanograms per deciliter (ng/dL), while females generally have levels between 15 to 70 ng/dL.
- Progesterone Levels: In women, progesterone levels fluctuate throughout the menstrual cycle, with typical ranges of 1 to 20 ng/mL during the luteal phase. In postmenopausal women, levels are often less than 0.5 ng/mL.
- Thyroid Function Tests: Normal ranges for Thyroid Stimulating Hormone (TSH) are generally between 0.4 to 4.0 milli-international units per liter (mIU/L).
- Complete Blood Count (CBC): Normal values for red blood cells, hemoglobin, and white blood cells can vary based on age and sex, making it essential to understand individual baselines.
Understanding these ranges helps patients and healthcare providers identify potential issues early. Deviations from the normal range can indicate that hormone therapy may need adjustment, either because levels are too low or too high.
When to Consult a Healthcare Provider
Patients undergoing hormone therapy should be vigilant about monitoring their symptoms and blood test results. Certain signs can indicate that hormone levels may be abnormal:
- Physical Symptoms: Unexplained weight gain or loss, fatigue, mood swings, or changes in libido can signal hormonal imbalances.
- Menstrual Irregularities: For women, changes in menstrual cycles, such as missed periods or heavy bleeding, may indicate a need for further evaluation.
- Mental Health Changes: Increased anxiety, depression, or irritability can also be linked to hormonal fluctuations.
If any of these symptoms are present, it’s essential to consult a healthcare provider. Open communication about symptoms and blood test results is vital for making informed treatment decisions. Providers may recommend additional tests or adjustments to therapy based on these discussions.
Making Adjustments to Therapy Based on Results
Adjustments to hormone therapy based on blood test results are common and necessary for optimal patient care. Here’s how healthcare providers typically approach this:
- Dosage Modifications: If blood tests show that hormone levels are too low, a healthcare provider may increase the dosage of the hormone being administered. Conversely, if levels are too high, they may reduce the dosage or change the delivery method.
- Switching Formulations: In cases where a particular hormone formulation isn’t yielding the desired results or is causing side effects, providers may consider switching to another type of hormone therapy or delivery method (e.g., from pills to patches or injections).
- Monitoring Frequency: Based on initial blood test results, healthcare providers may adjust the frequency of follow-up tests. For example, patients with significant fluctuations may require more frequent monitoring until levels stabilize.
Overall, the goal is to create an individualized treatment plan that aligns with the patient’s needs while minimizing risks and optimizing therapeutic benefits. Regularly interpreting blood test results and making necessary adjustments can greatly enhance the effectiveness of hormone therapy.
In the next section, we will discuss best practices for patients on hormone therapy, including how to prepare for blood tests and track symptoms effectively.
Best Practices for Patients on Hormone Therapy
Preparing for Blood Tests
Preparing for blood tests is essential for obtaining accurate results that inform hormone therapy management. Here are some tips for patients to consider:
- Timing Matters: Schedule blood tests at the appropriate time in relation to hormone administration. For example, if you’re on estrogen therapy, tests may be more accurate if taken just before your next dose or a specific time after administration, as directed by your healthcare provider.
- Follow Fasting Instructions: Some blood tests may require fasting for a certain period prior to testing. Always check with your healthcare provider about whether you should eat or drink before your blood test.
- Medication Awareness: Inform your healthcare provider about all medications and supplements you are taking, as some can influence hormone levels and test results. It’s important to know if you should skip any doses before testing.
- Stay Hydrated: Drink plenty of water before the test, as hydration can make it easier to draw blood and ensure accurate results.
- Relax: Anxiety can affect hormone levels, so try to remain calm before your test. Deep breathing techniques or light meditation can help ease pre-test jitters.
Keeping Track of Symptoms
Tracking symptoms is a vital part of hormone therapy. Here’s how to effectively monitor changes:
- Maintain a Symptom Diary: Keep a daily log of physical and emotional symptoms, noting any fluctuations, new symptoms, or changes in existing conditions. This diary will be invaluable during discussions with your healthcare provider.
- Record Menstrual Cycle Changes: For women, documenting menstrual cycle patterns can help identify irregularities that may warrant further investigation.
- Note Lifestyle Changes: Changes in diet, exercise, sleep, and stress levels can all impact hormone levels. Keeping track of these factors can provide context for any symptoms experienced.
- Use Technology: Consider using apps designed for tracking health symptoms. Many of these apps can help you log symptoms easily and even remind you of upcoming tests or appointments.
What to Expect During Monitoring
Understanding what to expect during the monitoring phase of hormone therapy can alleviate anxiety and promote effective communication with healthcare providers:
- Frequency of Blood Tests: Monitoring frequency varies based on individual treatment plans, but patients may expect tests every few weeks to months, particularly during the initial stabilization period. Once levels are stable, testing may reduce in frequency.
- Follow-Up Appointments: Regular follow-up appointments are crucial for discussing blood test results, adjusting dosages, and evaluating overall treatment efficacy. Be prepared to discuss your symptom diary during these visits.
- Communication is Key: Be open and honest with your healthcare provider about any symptoms, side effects, or concerns you may have. This feedback is crucial for tailoring your hormone therapy to your needs.
- Holistic Approach: Expect your healthcare provider to consider all aspects of your health during monitoring, including mental health, lifestyle, and any other medications or treatments you may be receiving.
Conclusion
In summary, the connection between hormone therapy and blood test monitoring is pivotal for achieving optimal health outcomes. Regular monitoring not only informs treatment adjustments but also empowers patients to take an active role in their healthcare journey. Engaging in open discussions with healthcare providers about symptoms and test results fosters a collaborative approach to managing hormone therapy effectively.
Disclaimer: This blog post is intended for educational purposes only and should not be taken as medical advice. Always consult your healthcare provider for personal health concerns.