National Overview
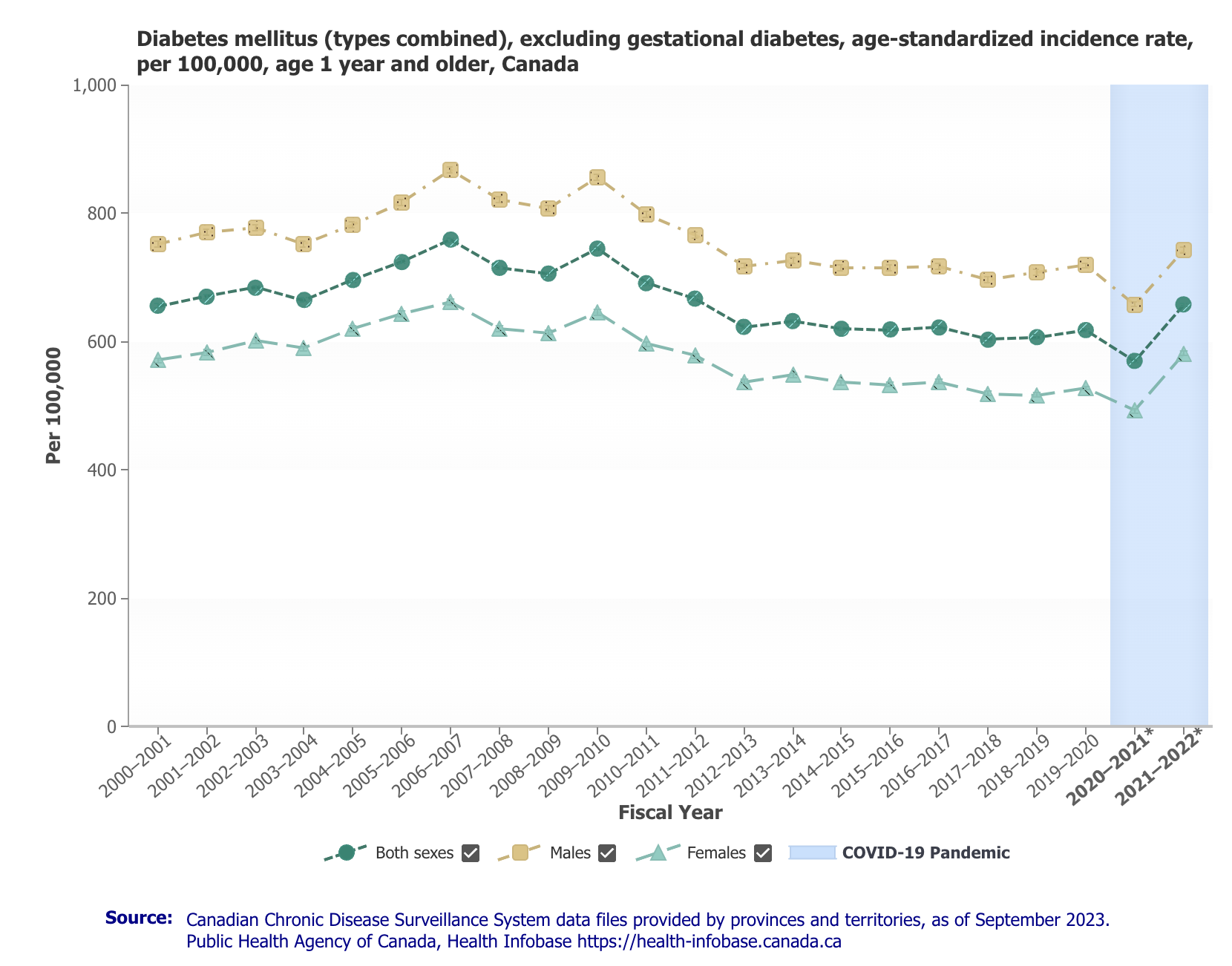
Over the past two decades, Canada has experienced a notable increase in diabetes incidence rates. The national average shows a general upward trend, particularly pronounced in older age groups. The incidence rate for the population aged 65 and above is significantly higher than for younger age groups. This increase can be attributed to factors such as aging population, sedentary lifestyles, and rising obesity rates.
In recent years, there appears to be a stabilization or slight decline in the national incidence rates. This could be indicative of improved public health initiatives, better disease management, and increased awareness about diabetes prevention.
Age Group Trends
[Embedded image: Diabetes Trends Canada by Age and Sex 2000-2022]
When breaking down the data by age groups, it is evident that the older population (65+) consistently exhibits the highest incidence rates. Middle-aged groups (45-64) also show significant increases, though not as high as the older age group. Younger age groups (under 20) have much lower incidence rates, though there is a slight upward trend over the years.
The high incidence rates in older age groups underscore the importance of targeted interventions for seniors, including lifestyle modifications, regular screenings, and effective management of pre-diabetes conditions.
Geographical Trends
[Embedded image: Diabetes Canada by Geograph 2000-2022]
Analyzing the data geographically reveals significant regional variations in diabetes incidence rates. Some provinces and territories deviate notably from the national trend:
- Newfoundland and Labrador, New Brunswick, and Manitoba: These regions exhibit significantly higher diabetes incidence rates compared to the national average. Factors contributing to these high rates may include regional lifestyle habits, socioeconomic factors, and access to healthcare services.
- Quebec: In contrast, Quebec shows a substantial negative deviation from the national trend, indicating lower incidence rates. This could be due to effective public health policies, better healthcare infrastructure, and preventive measures unique to the province.
- Other Regions: Provinces like Ontario, Alberta, and British Columbia have incidence rates that are relatively aligned with the national average. The territories such as Yukon and Nunavut show more variability, likely due to their smaller population sizes.
[Embedded image: Diabetes Trend 2000-2021 in Ontario]
[Embedded image: Diabetes Trend 2000-2021 in British Columbia]
[Embedded image: Diabetes Trend 2000-2021 in Alberta]
[Embedded image: Diabetes Trend 2000-2021 in Quebec]
[Embedded image: Diabetes Trend 2000-2021 in Manitoba]
[Embedded image: Diabetes Trend 2000-2021 in Prince Edward]
[Embedded image: Diabetes Trend 2000-2021 in Yukon]
[Embedded image: Diabetes Trend 2000-2021 in Saskatchewan]
[Embedded image: Diabetes Trend 2000-2021 in Nunavut]
[Embedded image: Diabetes Trend 2000-2021 in Nova Scotia]
[Embedded image: Diabetes Trend 2000-2021 in Labrador]
[Embedded image: Diabetes Trend 2000-2021 in New Brunswick]
Regional Analysis
- Newfoundland and Labrador: The highest positive deviation in diabetes incidence rates suggests that this region faces unique challenges. Possible factors include dietary habits, physical inactivity, and genetic predispositions. Public health strategies here may need to focus on community-specific interventions.
- Quebec: The significant negative deviation indicates that Quebec’s strategies in managing and preventing diabetes are effective. These might include robust public health campaigns, widespread availability of healthcare services, and possibly lower obesity rates compared to other regions.
- Nunavut and the Northwest Territories: These regions show variable trends, with Nunavut having a lower than average incidence rate. Challenges in these areas often relate to healthcare access, cultural differences in healthcare practices, and environmental factors.
Can Diabetes Be Reversed?
While Type 1 diabetes is currently considered an irreversible autoimmune condition, type 2 diabetes can be reversed in some individuals, especially if it’s caught early and managed effectively. The reversal of type 2 diabetes typically involves significant lifestyle changes that improve insulin sensitivity and reduce the body’s need for excessive insulin production. The main strategies to achieve this include:
- Weight loss: Losing weight, especially visceral fat around the abdomen, can improve insulin sensitivity and help the body regulate blood sugar levels better.
- Dietary changes: A diet low in processed carbohydrates and sugars, focusing on whole foods like vegetables, lean proteins, and healthy fats, can stabilize blood sugar levels.
- Regular physical activity: Exercise increases insulin sensitivity, helps with weight management, and can lower blood glucose levels.
- Intermittent fasting or caloric restriction: Some people have found that intermittent fasting or following very low-calorie diets can lead to remission of type 2 diabetes by reducing fat in the pancreas and liver.
- Medication adjustments: In some cases, medications like metformin or newer medications targeting insulin resistance or glucose production can help in reversing type 2 diabetes.
Reversing Insulin Resistance vs. Curing Diabetes
In type 2 diabetes, the pancreas may already have sustained damage to its insulin-producing cells, meaning that even if insulin sensitivity improves, the pancreas may not fully recover its ability to produce enough insulin. While blood sugar levels may return to normal, the underlying tendency toward insulin resistance often persists. This is why continued lifestyle management is crucial to maintaining these improvements. Many healthcare professionals prefer to use the term “remission” rather than “cure” when discussing diabetes improvement. Remission signifies that blood sugar levels have returned to normal without medication, yet the predisposition to diabetes remains, necessitating ongoing monitoring and the maintenance of healthy habits.
Conclusion
Diabetes trends in Canada reflect a complex interplay of demographic, socioeconomic, and regional factors. The overall increase in incidence rates, particularly among older age groups, highlights the growing public health burden. Regional disparities suggest that while some areas have successfully implemented effective diabetes management strategies, others lag and require more targeted interventions.
Addressing diabetes in Canada demands a multifaceted approach, involving improved healthcare access, community-specific health campaigns, lifestyle modification programs, and ongoing research into effective management and prevention strategies.
The rise of GLP-1 agonists like Ozempic offers a promising avenue for both the treatment and prevention of diabetes. By improving blood sugar control, promoting weight loss, and offering preventive benefits, these drugs have the potential to significantly reduce diabetes incidence rates in Canada. Their impact will likely be seen in the coming years as they become an integral part of diabetes management strategies.
Disclaimer: This blog post is intended for educational purposes only and should not be taken as medical advice. Always consult your healthcare provider for personal health concerns.