Section 1: Understanding Bone Density
Definition of Bone Density
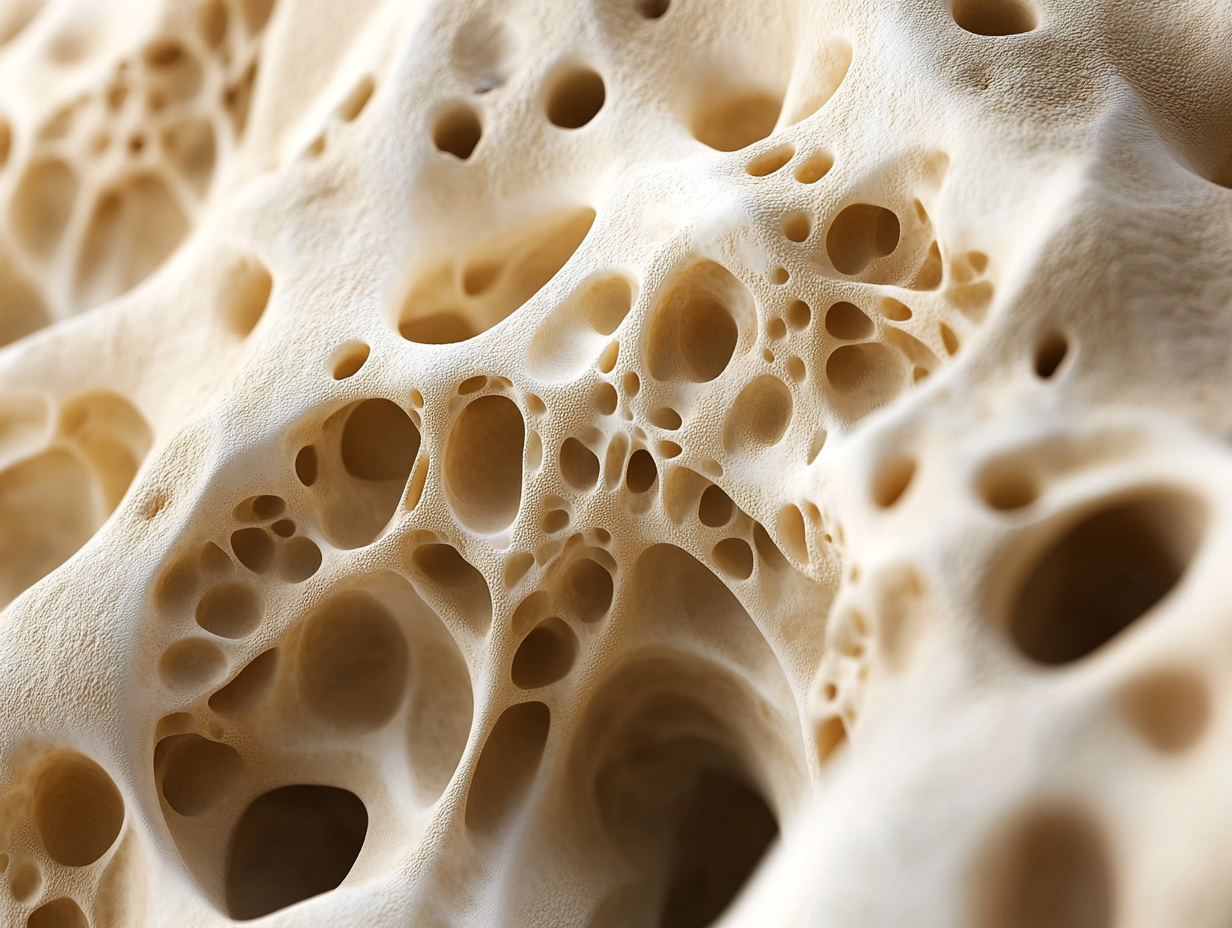
Bone density refers to the amount of mineral content (primarily calcium and phosphorus) present in a specific volume of bone. This measurement is crucial for assessing overall bone strength and health. Higher bone density typically indicates stronger bones that are less susceptible to fractures and other injuries, while lower bone density signifies weakened bones, which increases the risk of osteoporosis and related fractures. Understanding bone density is essential, particularly in aging populations where natural bone loss occurs over time.
Conditions Associated with Low Bone Density
Several medical conditions are commonly associated with low bone density, significantly impacting individuals' health and well-being. Osteoporosis is the most prevalent, characterized by a substantial decrease in bone density, leading to fragile bones that are prone to fractures even from minor falls. Osteopenia, a precursor to osteoporosis, indicates lower-than-normal bone density and requires monitoring and potential intervention to prevent progression to osteoporosis. Other conditions that can affect bone density include hyperthyroidism, certain autoimmune disorders, and long-term use of corticosteroids, all of which can compromise bone health and increase fracture risk.
Statistics on Bone Density Issues in Canada
Recent statistics reveal a concerning trend regarding bone density issues among Canadians. It is estimated that 1 in 3 women and 1 in 5 men aged 50 and older will experience a fracture due to osteoporosis in their lifetime. According to Osteoporosis Canada, over 2 million Canadians currently live with osteoporosis, a number projected to rise as the population ages. Furthermore, certain demographics, such as postmenopausal women and individuals with a family history of bone health issues, face an elevated risk. These statistics underscore the importance of awareness and proactive measures to address bone density concerns throughout the Canadian population, particularly as the aging demographic continues to grow.
By understanding the critical components of bone density and its associated conditions, individuals can better appreciate the importance of regular health assessments and the role of tools like blood tests in maintaining their skeletal health. In the next section, we will delve into how blood tests contribute significantly to bone health and the vital insights they provide into individual metabolic profiles.
Section 2: The Role of Blood Tests in Bone Health
Overview of Common Blood Tests
Blood tests are invaluable in assessing bone health and understanding the underlying factors that contribute to bone density issues. Several key markers are measured through these tests, each providing critical insights into an individual's skeletal health.
- Calcium Levels: Calcium is a fundamental mineral in bone formation and maintenance. A proper level of calcium in the blood is crucial as it reflects the body's ability to store and utilize this mineral for bone health. Low calcium levels may indicate dietary deficiencies or issues with absorption, necessitating a closer look at dietary intake and potential supplementation.
- Vitamin D Levels: Vitamin D plays a vital role in calcium absorption in the intestines and is essential for maintaining bone density. Insufficient levels of vitamin D can hinder calcium metabolism, leading to weakened bones and increased risk of fractures. In Canada, where sunlight exposure can be limited, particularly in winter, monitoring vitamin D levels is essential for promoting bone health.
- Parathyroid Hormone (PTH) Levels: The parathyroid hormone regulates calcium and phosphorus levels in the blood and plays a crucial role in bone metabolism. Elevated PTH levels can indicate that the body is trying to compensate for low calcium levels, which may lead to bone resorption where bones break down faster than they can be built up, resulting in decreased bone density.
- Alkaline Phosphatase: This enzyme is associated with bone turnover. Elevated levels of alkaline phosphatase can signal increased bone remodeling, which may be indicative of bone diseases such as Paget’s disease or conditions that increase bone loss. Monitoring this marker helps assess the dynamics of bone metabolism.
Insights into Bone Metabolism
By analyzing the results from these blood tests, healthcare providers can gain a deeper understanding of an individual's bone metabolism. Abnormal levels of calcium, vitamin D, PTH, or alkaline phosphatase can elucidate potential issues affecting bone density. For instance, low vitamin D and calcium levels, coupled with elevated PTH, might suggest a deficiency that could lead to weakened bones, while increased alkaline phosphatase may point towards active bone remodeling due to a pathological process.
Comprehensive blood testing provides a multi-faceted view of bone health, allowing for early detection of potential deficiencies or imbalances. This information is pivotal for designing targeted interventions and management strategies aimed at preventing further bone density loss and reducing fracture risk.
In the subsequent section, we will explore how abnormal blood test results can indicate bone density issues, the relationship between blood test findings and diagnostic imaging techniques such as DEXA scans, and include real-life case studies that highlight the effectiveness of early diagnosis through blood tests.
Section 3: How Blood Tests Indicate Bone Density Issues
Interpreting Abnormal Results
Abnormal blood test results can serve as critical indicators of underlying bone density issues. For example, low calcium and vitamin D levels are often interlinked with conditions such as osteoporosis and osteopenia. When calcium levels are low, the body may draw from the bones to maintain normal physiological functions, leading to a decrease in bone density over time.
Elevated parathyroid hormone (PTH) levels can signal that the body is reacting to low calcium levels, promoting bone resorption, in which bone tissue is broken down to release calcium into the bloodstream. This can lead to further bone density loss and heightened fracture risk. Similarly, increased alkaline phosphatase levels may indicate heightened bone turnover, suggesting that bone is being broken down faster than it can be built up, a concerning trend that merits investigation and intervention.
Interpreting these results requires a nuanced understanding of how these markers interact. For instance, a patient presenting with low vitamin D alongside elevated PTH may need supplementation and lifestyle adjustments to avert further complications, emphasizing the importance of early identification and intervention.
Connection to DEXA Scans
Blood test results can offer valuable context for interpreting DEXA (Dual-Energy X-ray Absorptiometry) scan outcomes, the gold standard for measuring bone mineral density. While blood tests highlight biochemical markers and potential deficiencies, DEXA scans provide a direct assessment of bone density at critical sites in the body, such as the hip and spine.
When healthcare providers receive abnormal blood test results, they may recommend DEXA scans to further evaluate the patient’s bone density. For example, if a blood test reveals low vitamin D levels, a DEXA scan can help assess whether this deficiency has led to decreased bone density. This holistic approach enables a more accurate diagnosis and aids in formulating a tailored treatment plan.
Case Studies
To illustrate the effectiveness of early diagnosis through blood tests, consider the following real-life case studies:
- Case Study 1: Jane's Journey Jane, a 68-year-old woman, visited her doctor for routine blood tests, during which low levels of vitamin D and calcium were identified. Concerned about her risk of osteoporosis, her physician recommended a DEXA scan, which confirmed a diagnosis of osteopenia. Jane was subsequently placed on a regimen of vitamin D and calcium supplements, along with lifestyle modifications, significantly bolstering her bone health and reducing her fracture risk.
- Case Study 2: Tom's Diagnosis Tom, a 72-year-old man, presented with unexplained fractures. Blood tests revealed elevated alkaline phosphatase and PTH levels, prompting further investigation. A DEXA scan revealed significant bone density loss, diagnosing him with osteoporosis. Recognizing the condition early allowed Tom's healthcare team to initiate treatment with bisphosphonates and lifestyle interventions, dramatically improving his outcomes.
These cases exemplify the pivotal role blood tests play in the early detection and management of bone density issues. Identifying abnormalities in blood work facilitates timely interventions, reducing the risk of more severe health complications and promoting overall skeletal health.
In the next section, we will delve deeper into additional diagnostic tools for assessing bone density, comparing the effectiveness of blood tests with imaging techniques like DEXA scans, and discussing subsequent steps based on initial testing outcomes.
Section 4: Additional Diagnostic Tools for Bone Density
Overview of DEXA Scans
DEXA (Dual-Energy X-ray Absorptiometry) scans are the most recommended method for assessing bone mineral density (BMD). This non-invasive imaging technique uses two different X-ray beams aimed at the bones to measure the amount of calcium and other minerals present. The scans are quick, typically taking only 10 to 30 minutes, and pose minimal radiation exposure to the patient.
During a DEXA scan, patients lie on a padded table while a scanning arm passes over their body to capture images. The results yield a T-score, which compares a patient's bone density with that of a healthy 30-year-old of the same sex. A T-score of -1.0 or above indicates normal bone density, between -1.0 and -2.5 signifies osteopenia (low bone density), and -2.5 or lower signals osteoporosis.
The DEXA scan results are vital for healthcare providers as they not only identify current bone health but also help in assessing fracture risk, guiding treatment options, and monitoring changes over time. With the context provided by blood tests, the results from a DEXA scan can lead to a comprehensive understanding of an individual’s bone health status.
Comparison of Blood Tests and Imaging Techniques
While both blood tests and imaging techniques like DEXA scans are essential in assessing bone health, they serve different purposes and have distinct advantages and limitations.
- Blood Tests:
- Pros:
- Provide insights into nutritional deficiencies and metabolic factors affecting bone density.
- Help in understanding the overall bone metabolism and biochemical activity that cannot be captured through imaging alone.
- They can predict the risk of potential bone density loss before it occurs, allowing for preventive measures.
- Cons:
- Blood tests do not directly measure bone density; rather, they suggest underlying issues that may affect bone health.
- Abnormalities in blood tests must be interpreted in the context of clinical presentation, which can sometimes lead to ambiguity.
- DEXA Scans:
- Pros:
- Offer a direct measurement of bone density, which is critical for diagnosing osteoporosis and osteopenia.
- Are the standard of care in monitoring treatment effectiveness and progression of bone density issues.
- Provide clear visual data that can facilitate patient understanding and engagement in their health management.
- Cons:
- DEXA scans require specialized equipment and trained personnel, which may not be accessible in all areas.
- They do not capture the biochemical factors influencing bone health, necessitating the need for accompanying blood tests.
In many cases, healthcare providers will use both blood tests and DEXA scans synergistically to develop a comprehensive picture of a patient's bone health. This dual approach ensures that both the chemical and structural aspects of bone density are evaluated, leading to more informed decision-making regarding treatment and prevention strategies.
Next Steps After Blood Tests
Upon receiving abnormal blood test results related to bone health, healthcare providers may recommend several next steps, which could include:
- Follow-Up Testing: Additional blood tests may be ordered to investigate specific abnormalities further, such as thyroid function tests or more specialized markers of bone metabolism, providing additional clarity regarding the patient’s bone health status.
- DEXA Scan Referral: In many cases, a DEXA scan will be recommended to assess current bone density. The information gained from the scan can confirm the presence of osteoporosis or osteopenia and guide treatment decisions.
- Personalized Treatment Plans: Based on the findings from blood tests and imaging, treatment strategies may be tailored for the individual. This might involve dietary changes, supplementation with calcium and vitamin D, initiation of medications such as bisphosphonates, or referrals to specialists like endocrinologists or nutritionists.
- Lifestyle Modifications: Patients may also receive counsel on modifying lifestyle factors that contribute to bone density issues, including dietary adjustments, exercise recommendations, and fall prevention strategies.
- Regular Monitoring: Depending on the severity of the findings, ongoing monitoring through regular blood tests and repeat DEXA scans may be required to track treatment effectiveness and adjust as necessary.
This proactive and comprehensive approach underscores the importance of utilizing both blood tests and imaging techniques to detect and manage bone density issues effectively, thereby improving patient outcomes and enhancing overall skeletal health.
In the next section, we will focus on prevention and management strategies to sustain and improve bone density, exploring actionable steps individuals can take to support their bone health across all life stages.
Section 5: Prevention and Management of Bone Density Issues
Tips for Healthy Bones
Maintaining optimal bone health is crucial, especially as individuals age or if they belong to at-risk populations for low bone density. Here are some actionable steps individuals can take to support their bone health:
- Balanced Diet:
- Calcium-Rich Foods: Incorporate dairy products such as yogurt, cheese, and milk, as well as non-dairy sources like leafy greens (kale, spinach), almonds, and fortified plant-based milk. Aim for a daily intake of 1,000 to 1,200 mg of calcium, depending on age and gender.
- Vitamin D Sources: Ensure adequate vitamin D levels through sun exposure, fortified foods, and fatty fish such as salmon and mackerel. Vitamin D is essential for calcium absorption and overall bone health; adults generally need about 600 to 800 IU per day.
- Protein Intake: Follow a balanced diet with sufficient protein, which plays a role in maintaining bone density. Great sources include lean meats, legumes, beans, and nuts.
- Regular Physical Activity:
- Engage in weight-bearing exercises such as walking, jogging, dancing, and resistance training, which help stimulate bone formation and maintain bone density. The Canadian Physical Activity Guidelines recommend at least 150 minutes of moderate-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days a week.
- Incorporate balance and flexibility exercises, such as yoga or tai chi, to prevent falls and related fractures.
- Avoiding Risks:
- Limit alcohol consumption, as excessive intake can lead to decreased bone density. The guideline for moderate drinking is defined as no more than two drinks per day for men and one drink for women.
- Quit smoking, as tobacco use is associated with decreased bone density and an increased risk of fractures.
- Regular Health Screenings:
- Schedule routine screenings and consultations with healthcare providers, especially for individuals over 50 or those with risk factors for osteoporosis. Regular blood tests and DEXA scans can help monitor bone health and allow for timely interventions.
Importance of Regular Screenings
Regular screenings for bone density issues are essential for early detection and intervention. The following points underline the significance of consistent monitoring:
- Identifying Changes Early: Routine blood tests and DEXA scans can help identify changes in bone density before serious problems develop, allowing for preventive measures to be taken well in advance.
- Tailoring Treatment Plans: Regular assessments enable healthcare providers to modify treatment plans based on the patient’s current bone health status. This may involve adjusting medication dosages, implementing new dietary recommendations, or initiating physical therapy.
- Informed Decision Making: Engaging in regular screenings empowers individuals with knowledge about their bone health, fostering proactive health management and decision-making.
Role of Healthcare Professionals
Healthcare professionals play an instrumental role in the prevention, diagnosis, and management of bone density issues. Their guidance can significantly impact overall bone health in the following ways:
- Comprehensive Assessments: Healthcare providers can conduct thorough evaluations, including medical history, lifestyle factors, and diagnostic tests to assess bone health accurately.
- Patient Education: Doctors and specialists can educate patients about the importance of bone health, risk factors for low bone density, and the necessary steps to improve and maintain bone strength.
- Personalized Treatment Plans: Based on the findings from blood tests and bone density assessments, healthcare professionals can create tailored treatment plans that may include medications, supplements, dietary changes, and exercise recommendations.
- Long-Term Support: Continuing support from healthcare providers can help individuals stay motivated and informed about their bone health journey, encouraging adherence to treatment and lifestyle recommendations.
In conclusion, focusing on prevention and management through healthy lifestyle choices, regular screenings, and collaboration with healthcare professionals can significantly improve bone density and overall skeletal health. The proactive steps taken today can lead to a healthier tomorrow, empowering individuals to maintain their mobility and quality of life as they age.
Conclusion
Throughout this article, we've explored the significance of bone density as a critical metric for skeletal health and overall wellness. Blood tests serve as essential tools for early detection of bone density issues, providing vital insights that pave the way for timely interventions.
We encourage readers to engage with their healthcare providers about their bone health and the importance of regular blood testing. Don't hesitate to ask questions or seek clarification about any concerns related to bone density.
Taking proactive steps to maintain and improve bone density is paramount. By understanding and implementing dietary guidelines, physical activity, and regular health screenings, individuals can foster a foundation for optimal bone health throughout all life stages.
Disclaimer: This blog post is intended for educational purposes only and should not be taken as medical advice. Always consult your healthcare provider for personal health concerns.